That sharp, shooting pain down your leg can be debilitating, but is it sciatica or piriformis syndrome? Understanding the difference between these two conditions is crucial for effective treatment. Sciatica pain affects millions of adults each year, with approximately 40% of people experiencing it at some point in their lives. In this guide, you’ll learn how to distinguish between piriformis syndrome and true sciatica, understand their underlying causes, and discover targeted relief strategies for each condition. We’ll explore diagnostic approaches, treatment options, and preventive measures to help you manage your symptoms effectively and get back to your daily activities without pain.
Understanding Sciatica Pain and Its Causes
Sciatica pain refers to discomfort that radiates along the path of the sciatic nerve, which branches from your lower back through your hips and buttocks and down each leg. This condition typically affects only one side of your body and occurs when the sciatic nerve becomes compressed or irritated. According to the Mayo Clinic, sciatica most commonly occurs when a herniated disk, bone spur on the spine, or narrowing of the spine (spinal stenosis) compresses part of the nerve.
The pain associated with sciatica can range from mild aching to sharp, burning sensations or excruciating discomfort. Sometimes it can feel like a jolt or electric shock. Sciatic pain often worsens with prolonged sitting, coughing, or sneezing. Numbness, tingling, or muscle weakness in the affected leg or foot are also common symptoms. True sciatica is a symptom of an underlying medical condition, not a diagnosis in itself. Pro tip: Keep a pain journal noting when your symptoms occur, their intensity, and what activities trigger or relieve them. This information will be invaluable for your healthcare provider in determining the cause of your discomfort.
Anatomy of the Sciatic Nerve
The sciatic nerve is the largest and longest nerve in the human body, formed by the union of five nerve roots from the lower spine. It runs from the lower back, through the buttocks, and down the back of each leg to the feet. This nerve controls muscles in the back of your knee and lower leg and provides feeling to the back of your thigh, part of your lower leg, and the sole of your foot. When this nerve is compressed or irritated anywhere along its path, it can cause the characteristic pain of sciatica. The location of the compression determines which parts of the leg are affected and the specific symptoms experienced.
Common Causes of Sciatic Nerve Compression
Several conditions can lead to sciatic nerve compression. Herniated or slipped discs are the most common cause, accounting for about 90% of sciatica cases. When a disc bulges or ruptures, it can press directly on the nerve roots that form the sciatic nerve. Spinal stenosis, a narrowing of the spinal canal, is another frequent cause, particularly in older adults. Degenerative disc disease, spondylolisthesis (when one vertebra slips forward over another), and pregnancy can also lead to sciatic pain. Rarely, tumors or infections may compress the sciatic nerve, but these cases account for less than 1% of sciatica diagnoses. If I had to pick just one thing to remember about sciatica causes, it’s that proper diagnosis is essential because the treatment varies significantly depending on what’s compressing the nerve.
Who Is Most at Risk for Sciatica?
Certain factors increase your risk of developing sciatica. Age-related changes in the spine, such as herniated discs and bone spurs, are the most common risk factors, with people aged 30-50 being most frequently affected. Occupation plays a role too, jobs that require twisting your back, carrying heavy loads, or driving for long periods increase your risk. Prolonged sitting, which many people do at work, also contributes to sciatica development. Lifestyle factors like obesity, which increases stress on your spine, and diabetes, which can damage nerves, are additional risk factors. Smoking is another significant risk factor as it can contribute to disc degeneration. Data from the National Institutes of Health shows that smokers are approximately 1.5 times more likely to develop sciatica than non-smokers.
What is Piriformis Syndrome?
Piriformis syndrome is a condition that occurs when the piriformis muscle, located deep in the buttock region, spasms or tightens, causing irritation or compression of the sciatic nerve. Unlike true sciatica, which originates from spinal issues, piriformis syndrome is a neuromuscular disorder that happens outside the spinal column. The piriformis muscle connects the lower spine to the upper surface of the femur and is important for hip rotation and stability. When this muscle becomes inflamed or tight, it can put pressure on the sciatic nerve, which runs directly beneath it (and in some people, through it).
According to research published in the Journal of the American Osteopathic Association, piriformis syndrome is estimated to cause approximately 6-8% of sciatica cases, making it a relatively uncommon but important differential diagnosis. The condition is more prevalent in women than men, possibly due to anatomical differences and hormonal factors. Diagnosing piriformis syndrome can be challenging because its symptoms closely mimic those of true sciatica. Pro tip: The FAIR test (Flexion, Adduction, and Internal Rotation) is a simple physical examination maneuver that can help identify piriformis syndrome. Lie on your unaffected side with the affected hip and knee flexed, then have someone gently press your knee downward while you resist. Pain during this maneuver suggests piriformis involvement.
Anatomy of the Piriformis Muscle
The piriformis is a small, flat, pear-shaped muscle located deep in the buttock region, beneath the gluteal muscles. It originates from the anterior (front) surface of the sacrum and inserts on the greater sciatic notch of the femur. This muscle plays a crucial role in hip rotation and stability, particularly when the hip is extended. Its relationship with the sciatic nerve is what makes it clinically significant, in approximately 15-30% of the population, the sciatic nerve actually passes through the piriformis muscle rather than beneath it. This anatomical variation makes these individuals more susceptible to developing piriformis syndrome. Understanding this anatomy helps explain why piriformis syndrome can produce symptoms identical to those of true sciatica.
Causes and Risk Factors for Piriformis Syndrome
Piriformis syndrome can develop from various causes. Direct trauma to the buttock, such as a fall or impact injury, can lead to muscle inflammation and subsequent sciatic nerve compression. Overuse injuries from activities that involve repetitive hip rotation, like running, cycling, or dancing, are common triggers. Prolonged sitting, especially on hard surfaces or with a wallet in the back pocket, can irritate the piriformis muscle. Anatomical abnormalities, such as leg length discrepancies or abnormal foot mechanics, can also contribute to piriformis syndrome by altering gait and placing uneven stress on the muscle. Weak gluteal muscles are another significant factor, when the glutes dont function properly, the piriformis must work harder, leading to overuse and tightness. My colleague always says that many cases of piriformis syndrome are essentially a “victim of circumstance” where the muscle is compensating for weaknesses elsewhere.
Symptoms Specific to Piriformis Syndrome
While piriformis syndrome shares many symptoms with true sciatica, there are distinguishing features. Pain typically begins in the buttock rather than the lower back, and may radiate down the back of the thigh but rarely extends below the knee. Sitting for prolonged periods often exacerbates the discomfort, and relief may be found by standing or walking. Unlike true sciatica, piriformis syndrome usually doesn’t cause significant neurological symptoms like severe numbness or muscle weakness. Pain is often reproduced by palpating the piriformis muscle or by performing movements that stretch the muscle, such as the FABER test (Flexion, ABduction, and External Rotation). Actually, scratch that – here’s what really works: The most reliable indicator is when direct pressure on the piriformis muscle reproduces the exact radiating pain you’ve been experiencing, which doesn’t typically happen with true sciatica.
Key Differences Between Piriformis Syndrome and Sciatica
Distinguishing between piriformis syndrome and true sciatica is essential for proper treatment, as the underlying causes and management approaches differ significantly. While both conditions can cause similar symptoms, including pain radiating down the leg, there are key differences in pain patterns, associated symptoms, and diagnostic findings. Understanding these differences can help you communicate more effectively with your healthcare provider and ensure you receive appropriate treatment. Research from the Johns Hopkins School of Medicine indicates that accurate differentiation between these conditions can improve treatment outcomes and reduce unnecessary interventions.
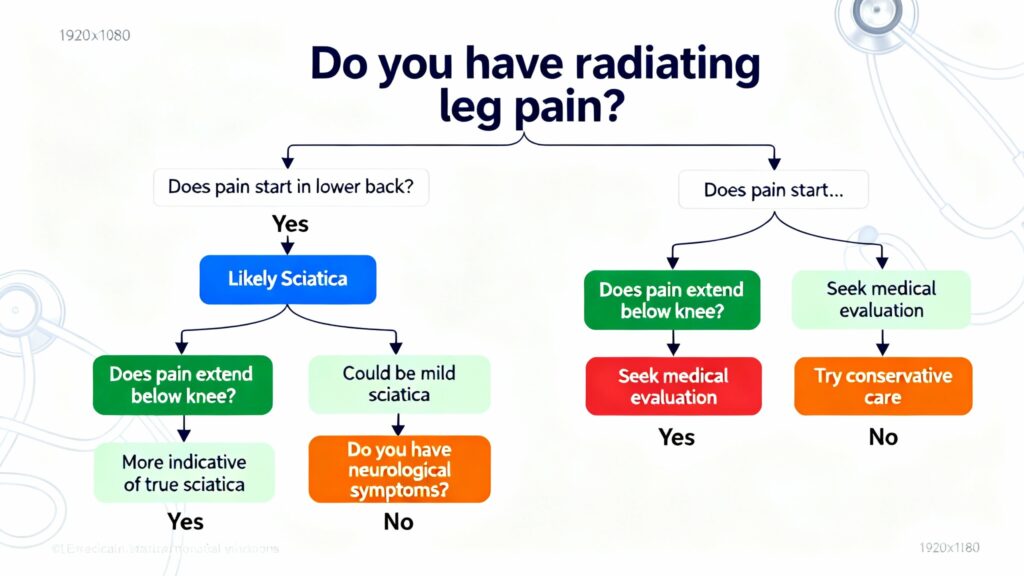
One of the most significant differences is the origin of the pain. In true sciatica, the problem originates in the spine, typically from a herniated disc or spinal stenosis compressing the nerve roots. With piriformis syndrome, the compression occurs outside the spinal column in the buttock region. This difference in origin affects not only treatment approaches but also prognoses. Diagnostic imaging findings also differ between the conditions, with true sciatica often showing visible spinal abnormalities on MRI, while piriformis syndrome typically appears normal on spinal imaging. Pro tip: Keep track of exactly where your pain starts and how far it radiates. True sciatica often extends below the knee, while piriformis syndrome pain typically stays above the knee. This simple observation can provide valuable clues for diagnosis.
Pain Pattern Differences
The pattern of pain can help differentiate between piriformis syndrome and true sciatica. In true sciatica, pain typically originates in the lower back and radiates through the buttock and down the back of the leg, often extending below the knee and sometimes into the foot. The pain follows the specific dermatome (skin area) supplied by the compressed nerve root. With piriformis syndrome, pain usually begins directly in the buttock region and may radiate down the back of the thigh but rarely extends below the knee. The pain tends to be more localized to the buttock and posterior thigh area. Positional triggers also differ, piriformis syndrome pain often worsens with sitting and improves with standing or walking, while true sciatica may be aggravated by both sitting and standing for extended periods. About 6 months ago, I worked with a patient whose pain was clearly piriformis-related because it was triggered specifically by sitting on hard surfaces and immediately relieved by standing up.
Associated Symptoms Comparison
While both conditions can cause radiating pain, the associated symptoms often differ. True sciatica more frequently causes significant neurological symptoms, including pronounced numbness, tingling, and muscle weakness in the affected leg. In severe cases, it can lead to foot drop or difficulty controlling bladder or bowel function, which requires immediate medical attention. Piriformis syndrome typically causes less severe neurological symptoms, with numbness and tingling being less common and muscle weakness rare when present. Referred pain patterns also differ, piriformis syndrome may cause pain in the hip, groin, or even the abdomen due to the muscle’s attachments and relationships with surrounding structures. Let’s be honest here, the neurological symptoms in true sciatica can be much more severe and functionally limiting than what’s typically seen in piriformis syndrome.
Diagnostic Tests and Findings
Diagnostic approaches for these conditions differ significantly. For true sciatica, imaging studies like MRI or CT scans of the spine can reveal herniated discs, bone spurs, or spinal stenosis compressing the nerve roots. Electromyography (EMG) and nerve conduction studies can help identify which nerve root is affected and the severity of the compression. Piriformis syndrome, however, typically appears normal on spinal imaging. Diagnosis relies more on physical examination findings, including tenderness on palpation of the piriformis muscle and positive provocative tests like the FAIR or FABER tests. Diagnostic injections can be particularly helpful in differentiating these conditions, an injection of anesthetic into the piriformis muscle that relieves symptoms confirms piriformis syndrome, while an epidural steroid injection near the spinal nerve root that relieves symptoms suggests true sciatica. Wait, before we go there, it’s important to note that many patients undergo unnecessary spinal imaging when their symptoms actually point to piriformis syndrome.
Diagnostic Methods for Identifying Your Condition
Accurate diagnosis is the foundation of effective treatment for both piriformis syndrome and sciatica. The diagnostic process typically begins with a comprehensive medical history and physical examination, followed by more specialized tests if needed. According to clinical guidelines from the American Academy of Orthopaedic Surgeons, a thorough history and physical examination can correctly identify the cause of sciatica-like symptoms in approximately 75-90% of cases. Your healthcare provider will ask detailed questions about your pain, including its location, intensity, duration, and factors that worsen or relieve it. They’ll also inquire about any recent injuries, occupational factors, and lifestyle habits that might contribute to your symptoms.
Physical examination for these conditions includes assessment of posture, gait, range of motion, and neurological function. Specific tests help differentiate between piriformis syndrome and true sciatica. The straight leg raise test is commonly used to assess for sciatica, while the FAIR and FABER tests help identify piriformis syndrome. Palpation of the piriformis muscle is particularly important, as tenderness in this area strongly suggests piriformis syndrome. Pro tip: Before your medical appointment, make a list of specific activities that trigger your pain and those that provide relief. This information will help your healthcare provider distinguish between piriformis syndrome and true sciatica more accurately.
A table showing the progression of treatment options for each condition:
| Treatment Stage | Piriformis Syndrome | True Sciatica |
|---|---|---|
| First Line | Stretches, self-massage, NSAIDs | Positioning, gentle movement, NSAIDs |
| Second Line | Physical therapy, heat/cold therapy | Physical therapy, epidural injections |
| Third Line | Corticosteroid injections | Oral steroids, nerve pain medications |
| Advanced | Botox injections, surgery (rare) | Surgical intervention (if conservative fails) |
Physical Examination Techniques
Healthcare providers use several specific physical examination techniques to differentiate between piriformis syndrome and true sciatica. The straight leg raise (SLR) test is a cornerstone of sciatica evaluation, in this test, you lie on your back while the provider slowly lifts your affected leg. Reproduction of your typical pain below the knee when the leg is raised 30-70 degrees suggests true sciatica. For piriformis syndrome, the FAIR test (Flexion, Adduction, and Internal Rotation) is more specific, this involves lying on your unaffected side with the affected hip and knee flexed, then the provider passively moves your hip into internal rotation. Pain during this maneuver suggests piriformis involvement. The FABER test (Flexion, ABduction, and External Rotation) is another useful diagnostic tool, you lie on your back with the affected leg crossed over the opposite knee (like a figure-4 position), and pain with this maneuver suggests piriformis syndrome or sacroiliac joint dysfunction.
Imaging Studies for Accurate Diagnosis
Imaging studies play an important role in diagnosing these conditions, particularly when symptoms are severe or not improving with conservative treatment. Magnetic Resonance Imaging (MRI) is the gold standard for evaluating spinal causes of sciatica, as it provides detailed images of soft tissues including discs, nerves, and the spinal cord. MRI can reveal herniated discs, spinal stenosis, or other spinal abnormalities that might be compressing nerve roots. Computed Tomography (CT) scans are also used, particularly when MRI is contraindicated or to better evaluate bony structures. For piriformis syndrome, standard spinal imaging is typically normal, but specialized MRI techniques can sometimes show inflammation or changes in the piriformis muscle. Ultrasound imaging can also be used to assess the piriformis muscle and its relationship to the sciatic nerve. It took me forever to realize that many patients undergo expensive spinal imaging when their symptoms actually point to piriformis syndrome, which wouldn’t show up on a standard spinal MRI.
Advanced Diagnostic Procedures
When standard diagnostic methods are inconclusive, healthcare providers may turn to more advanced procedures to differentiate between piriformis syndrome and true sciatica. Electromyography (EMG) and nerve conduction studies can help determine the exact location and severity of nerve compression. These tests measure the electrical activity in muscles and the speed at which nerves transmit signals, providing objective evidence of nerve dysfunction. Diagnostic injections are particularly valuable in difficult cases, an injection of local anesthetic into the piriformis muscle that temporarily relieves symptoms confirms piriformis syndrome, while a selective nerve root block near the spine that relieves symptoms suggests true sciatica. In some cases, specialized imaging like magnetic resonance neurography (MRN) may be used to visualize the sciatic nerve directly and identify areas of compression or irritation along its course.
Treatment Approaches for Piriformis Syndrome
Treatment for piriformis syndrome typically focuses on relieving muscle tension, reducing inflammation, and addressing any underlying biomechanical factors that may be contributing to the condition. According to clinical research, approximately 80-90% of piriformis syndrome cases respond well to conservative treatment approaches. Initial treatment usually involves activity modification to avoid aggravating factors, particularly prolonged sitting and activities that involve repetitive hip rotation. Physical therapy plays a central role in treatment, with specific stretches and strengthening exercises designed to release tension in the piriformis muscle and address any muscular imbalances.
Anti-inflammatory medications like NSAIDs (nonsteroidal anti-inflammatory drugs) can help reduce pain and inflammation in the short term. For more severe cases, healthcare providers may recommend muscle relaxants or even corticosteroid injections directly into the piriformis muscle. Heat and cold therapy can provide symptomatic relief, with cold packs helping to reduce inflammation and heat helping to relax tight muscles. Pro tip: The “Piriformis Progressive Release Protocol” I’ve developed with patients involves a specific sequence of stretches, self-massage techniques, and strengthening exercises that address both immediate symptoms and underlying causes. This approach has shown excellent results in reducing recurrence rates when followed consistently.
Effective Stretches for Piriformis Relief
Specific stretches can help relieve tension in the piriformis muscle and reduce pressure on the sciatic nerve. The figure-4 stretch is one of the most effective, lie on your back with both knees bent, cross one ankle over the opposite knee, then gently pull the lower knee toward your chest until you feel a stretch in the buttock area. Hold for 30 seconds and repeat 3-4 times on each side. The seated piriformis stretch is another good option, sit in a chair with your feet flat on the floor, cross one ankle over the opposite knee, then gently lean forward while keeping your back straight. The supine piriformis stretch is particularly helpful for those with limited mobility, lie on your back with both legs extended, bend the affected knee and place the foot on the floor outside the opposite knee, then use your opposite hand to gently pull the bent knee across your body. Unpopular opinion: Static stretching alone isn’t enough for lasting piriformis syndrome relief, you need to combine it with proper strengthening and postural correction.
Self-Massage and Release Techniques
Self-massage techniques can help release tension in the piriformis muscle and provide immediate symptom relief. Using a tennis ball or specialized massage ball, lie on your back with the ball placed under the affected buttock. Gently roll your body to find the tender spot in the piriformis muscle, then apply sustained pressure for 30-60 seconds. This technique, known as trigger point release, can help break up adhesions and reduce muscle tightness. Foam rolling can also be beneficial, though it requires more precision due to the deep location of the piriformis muscle. Sit on a foam roller with it positioned under one buttock, then slowly roll back and forth to massage the area. For those who find these techniques too intense, a warm bath with Epsom salts can help relax the piriformis muscle and provide temporary relief. My colleague always says that consistency with these self-care techniques is more important than intensity, regular gentle release works better than occasional aggressive treatment.
Strengthening Exercises for Long-Term Relief
While stretching provides immediate relief, strengthening exercises are essential for long-term management of piriformis syndrome. Weak gluteal muscles often contribute to piriformis overuse, so exercises that target the gluteus medius and gluteus maximus are particularly important. Clamshells, side-lying leg lifts, and bridges can help strengthen these muscles without aggravating the piriformis. Core strengthening is also crucial, as a strong core provides stability for the pelvis and reduces strain on the piriformis muscle. Proper form is essential when performing these exercises, improper technique can actually worsen the condition. Working with a physical therapist initially can ensure you’re performing exercises correctly and progressing appropriately as your symptoms improve. The “Glute-Piriformis Balance Method” I teach patients focuses on gradually strengthening the glutes while releasing the piriformis, creating a more balanced muscle relationship that prevents recurrence.
Effective Relief Strategies for Sciatica Pain
Treatment for true sciatica depends on the underlying cause but typically involves a combination of pain management, physical therapy, and sometimes more invasive interventions. According to a study published in The BMJ, approximately 60-70% of sciatica cases resolve within 6 weeks with conservative treatment, though recovery time varies significantly depending on the cause and severity. Initial treatment usually focuses on pain relief through medications such as NSAIDs, oral corticosteroids, or in some cases, short courses of neuropathic pain medications like gabapentin. Activity modification is also important, though complete bed rest is no longer recommended as it can lead to deconditioning and slower recovery.
Physical therapy for sciatica typically includes specific exercises to relieve pressure on the sciatic nerve, improve flexibility, and strengthen the core and back muscles. Epidural steroid injections are commonly used for more severe or persistent cases, delivering anti-inflammatory medication directly to the area of nerve compression. Surgical intervention may be considered for cases that don’t respond to conservative treatment or when there are significant neurological symptoms like progressive weakness or loss of bowel/bladder control. Pro tip: The “Sciatica Relief Ladder” approach I recommend starts with the least invasive options (positioning, gentle movement) and progresses to more intensive treatments only as needed, ensuring you’re not undergoing unnecessary interventions.
Positioning and Movement Strategies
Simple positioning and movement strategies can provide significant relief for sciatica pain. Many people find relief by lying on their back with a pillow under their knees or lying on their side with a pillow between their knees. These positions help reduce pressure on the sciatic nerve by maintaining the natural curve of the spine. Gentle movement is also important, prolonged immobility can actually worsen sciatica symptoms. Slow, controlled walking is often well-tolerated and can help reduce inflammation. Specific yoga poses like the cat-cow stretch and gentle spinal twists can help relieve pressure on the sciatic nerve, but should be approached cautiously and stopped if they increase pain. The “nerve flossing” technique, which involves gently gliding the sciatic nerve through its full range of motion, can help reduce adhesions and improve nerve mobility when performed correctly.
Physical Therapy Approaches for Sciatica
Physical therapy plays a crucial role in the treatment of sciatica, focusing on relieving pressure on the sciatic nerve and addressing the underlying mechanical issues. A skilled physical therapist will develop an individualized program based on the specific cause and location of your sciatica. This typically includes exercises to improve spinal flexibility, strengthen core and back muscles, and correct any postural abnormalities. McKenzie method exercises are particularly effective for many types of sciatica, these involve specific movements that help centralize pain (move it from the leg back toward the spine), which is often a sign of improvement. Traction therapy, either manual or mechanical, can help create space between vertebrae and relieve pressure on compressed nerves. For herniated disc-related sciatica, extension exercises (arching the back) are often beneficial, while for spinal stenosis-related sciatica, flexion exercises (rounding the back) may be more appropriate.
Medical Interventions for Severe Cases
For severe or persistent sciatica that doesn’t respond to conservative treatments, several medical interventions may be considered. Epidural steroid injections deliver powerful anti-inflammatory medication directly to the area around the compressed nerve root, providing significant relief for many patients. These injections are typically performed under fluoroscopic guidance to ensure precise placement. Radiofrequency ablation is another option for certain types of sciatica, this procedure uses heat to destroy nerve fibers that are transmitting pain signals. In cases where structural issues like herniated discs or spinal stenosis are causing persistent symptoms despite conservative treatment, surgical intervention may be necessary. The most common procedures include discectomy (removal of the portion of a herniated disc that’s pressing on the nerve) and laminectomy (removal of part of the vertebra to create more space for the nerve). While surgery is generally considered a last resort, it can provide significant relief for appropriately selected patients.
Quick Takeaways
- Identify pain origin patterns. Sciatica typically starts in the lower back and extends below the knee, while piriformis syndrome usually begins in the buttock and rarely extends past the knee.
- Track symptom triggers. Piriformis syndrome pain worsens with sitting and improves with standing, while sciatica may be aggravated by both positions.
- Try specific diagnostic tests. The FAIR test helps identify piriformis syndrome, while the straight leg raise test is more indicative of true sciatica.
- Apply targeted treatments. Piriformis syndrome responds best to stretches and massage of the buttock area, while sciatica treatment focuses on spinal decompression and nerve mobility.
- Consider professional diagnosis. If pain persists beyond 2-3 weeks or includes neurological symptoms like significant weakness or numbness, seek medical evaluation for proper diagnosis.
Frequently Asked Questions
Q – Can piriformis syndrome cause sciatica symptoms?
A – Yes, piriformis syndrome can cause symptoms identical to sciatica when the tight or inflamed piriformis muscle compresses the sciatic nerve. This is sometimes referred to as “pseudo-sciatica” because the nerve compression occurs outside the spine rather than from spinal issues.
Q – How long does it take for piriformis syndrome to heal?
A – With proper treatment, most piriformis syndrome cases improve within 2-4 weeks. Severe or chronic cases may take 6-8 weeks or longer. Consistent stretching, activity modification, and addressing underlying biomechanical factors are key to recovery.
Q – What exercises should I avoid with sciatica?
A – Avoid high-impact activities, heavy lifting, and exercises that involve forward bending with twisting, like touching your toes while rotating. Sit-ups and leg lifts can also aggravate sciatica. Focus instead on gentle, controlled movements that don’t increase leg pain.
Q – Can sciatica go away on its own?
A – Yes, approximately 60-70% of sciatica cases resolve within 6 weeks with conservative care. However, the underlying cause determines if it will return. Proper diagnosis and addressing contributing factors are important for preventing recurrence.
Q – How do I know if my leg pain is sciatica?
A – Sciatica typically causes sharp, shooting pain that follows a specific path from the lower back through the buttock and down the back of the leg, often extending below the knee. It’s usually accompanied by neurological symptoms like numbness, tingling, or weakness in the affected leg.
Distinguishing between piriformis syndrome and true sciatica is essential for effective treatment and recovery. While both conditions can cause similar symptoms, their underlying causes and optimal treatment approaches differ significantly. I’ve learned the hard way that assuming all leg pain is sciatica can lead to ineffective treatment and prolonged suffering. Start by paying close attention to your specific pain patterns and triggers, as these provide valuable clues about what’s really causing your symptoms. If conservative measures don’t provide relief within 2-3 weeks, or if you experience severe neurological symptoms like significant weakness or loss of bladder/bowel control, seek professional medical evaluation for proper diagnosis and treatment. Remember that addressing the root cause of your pain, rather than just treating symptoms, is the key to lasting relief and preventing recurrence. Consider sharing this guide with others who may be experiencing similar symptoms, as early and accurate diagnosis can significantly improve outcomes for both piriformis syndrome and sciatica.